Fix My Flat Foot
Our flat foot correction plans combine advanced gait analysis, bespoke orthoses and minimally invasive surgery where appropriate. We tailor every approach to reduce pain, improve arch support and restore confident movement.
- Comprehensive biomechanics assessment and imaging
- Custom orthotics & strengthening programmes
- Specialist surgical options for severe deformity
You'll receive a clear treatment map, from conservative therapy through to recovery milestones after surgery. Our multidisciplinary team supports you through every stage.
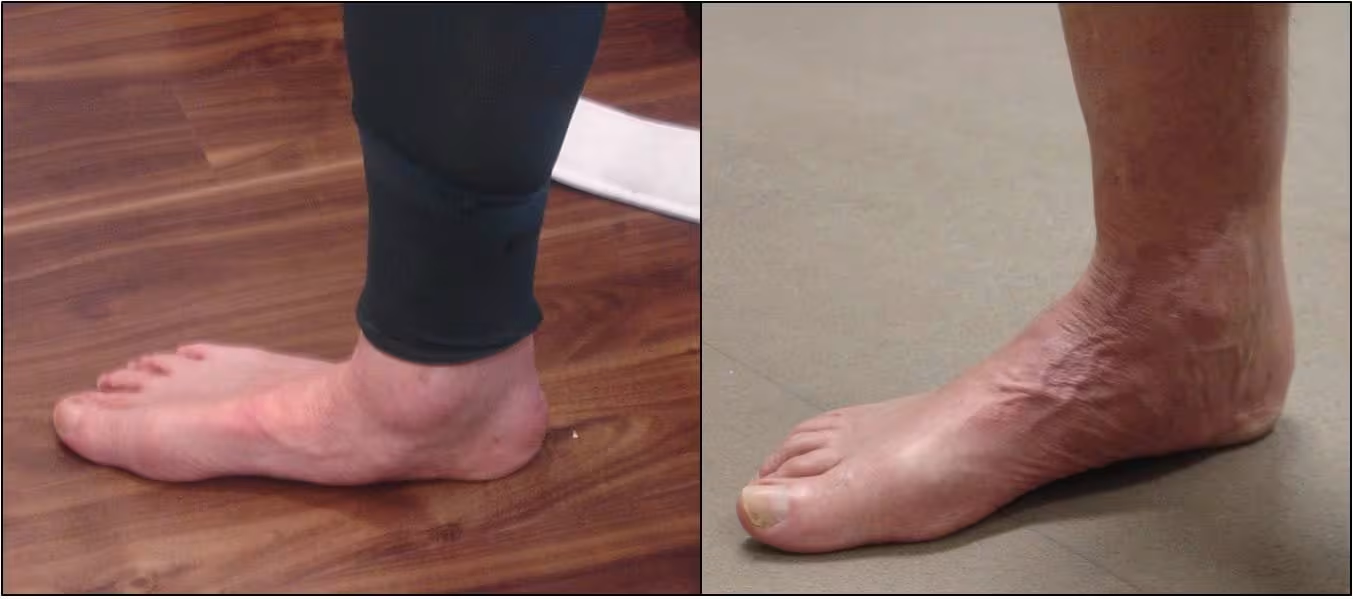

Flat Foot Correction at the Foot & Ankle Centre provides advanced, personalised treatment for patients experiencing pain, fatigue, or mobility issues caused by fallen arches or overpronation. Flat feet can lead to ankle and knee discomfort, difficulty walking long distances, and increased strain on tendons such as the posterior tibial tendon.
Our specialist surgeons and clinicians offer a full range of non-surgical and surgical solutions tailored to your foot structure and lifestyle. Non-surgical treatments may include custom orthotics, physiotherapy, bracing, and targeted strengthening programmes. For cases where conservative care is not effective, we provide state-of-the-art surgical correction techniques—including tendon reconstruction, calcaneal osteotomy (heel realignment), and minimally invasive procedures—to restore proper arch support and improve long-term biomechanics.
At the Foot & Ankle Centre, we use advanced imaging, gait analysis, and modern corrective techniques to ensure safe, effective, and lasting relief. Our goal is to realign the foot, reduce pain, and help you return to a comfortable, active lifestyle.
FAQs
Flat foot is a condition where the arch collapses and the entire sole rests on the ground. It may be present from childhood or develop due to tendon weakness, injury, arthritis, or biomechanics.
Symptoms include arch or heel pain, tired or achy feet, ankle or knee discomfort, rolling inwards (overpronation), difficulty standing or walking long durations, and uneven shoe wear. If symptoms persist, an assessment is recommended.
Causes can include genetics, posterior tibial tendon dysfunction, injury, arthritis, ligament weakness, or poor footwear. Some cases are flexible and painless; others progressively worsen.
Diagnosis involves physical examination, gait analysis, and imaging such as X-rays or ultrasound to determine severity, cause, and the right treatment path.
Custom orthotics, physiotherapy and strengthening programmes, footwear modifications, bracing for tendon support, and anti-inflammatory treatments. Many patients improve without surgery.
Surgery may be needed for persistent pain, tendon damage progression, severe deformity, or when conservative care no longer works.
Options include tendon reconstruction (e.g., posterior tibial tendon), calcaneal osteotomy (heel realignment), spring ligament repair, fusion procedures for advanced arthritis, and minimally invasive corrections. Your surgeon tailors the approach.
Typical recovery: 6–8 weeks protected weight-bearing in a boot; 8–12 weeks gradual return to walking; 3–6 months increasing activity; 6–12 months for full recovery. A personalised rehab plan is provided.
Yes. Correcting the deformity restores alignment, reduces strain on joints and tendons, and improves comfort for daily activities and exercise.
Contact the Foot & Ankle Centre through our website, phone, or online enquiry form to arrange an assessment and personalised plan.